Delusions in psychology are beliefs that persist despite evidence to the contrary. They are often associated with mental illnesses such as schizophrenia, bipolar disorder, or severe depression. Delusions can encompass a wide range of topics and are resistant to logical reasoning or contradictory evidence.
People with delusions may believe that they are being persecuted, monitored, or controlled by external forces or that they have special abilities or powers. These beliefs can be distressing and disruptive to daily life. Treatment may include therapy and medication to manage symptoms and improve overall well-being.
Delusions could result from misinterpreting events, or they may involve some level of paranoia.
Delusions can be either bizarre or non-bizarre. Bizarre delusions are characterized as beliefs about something that can never happen, e.g., the belief that an individual has been abducted and cloned by aliens.
Non-bizarre delusions, however, are beliefs that could be true, such as the belief that an individual is being stalked, that someone is in love with them, or a spouse is cheating on them.
What is Delusional Disorder?
Delusional disorder is a condition characterized by persistent non-bizarre delusions lasting at least one month (Joseph & Siddiqui, 2023). These reality-impairing beliefs could feasibly occur in real life but remain firmly held despite evidence to the contrary. Unlike hallucinations in schizophrenia, no other psychotic symptoms are present.
People diagnosed with delusional disorder can experience realistic delusions, such as believing they are being deceived or conspired against, but these are usually highly exaggerated or untrue.
Often, with delusional disorder, the individual will socialize and function according to social norms and generally does not behave unusually, making this condition difficult to recognize from an outsider’s perspective.
Delusional disorder, therefore, differs from other psychotic disorders where delusions are present, such as schizophrenia, as there are other symptoms of those conditions that can affect the functioning of those individuals.
Delusional disorder affects around 0.02% of the population across their lifetime (Kalayasiri et al., 2019). Onset often occurs in middle age with prevalence peaking between ages 40-49, though cases exist from young adulthood to old age.
Particular delusion types show gender differences, like erotomanic delusions being more common among women and persecutory and jealous delusions among men.
Types of delusions
Many different types of delusions can be experienced, characterized by delusional disorder.
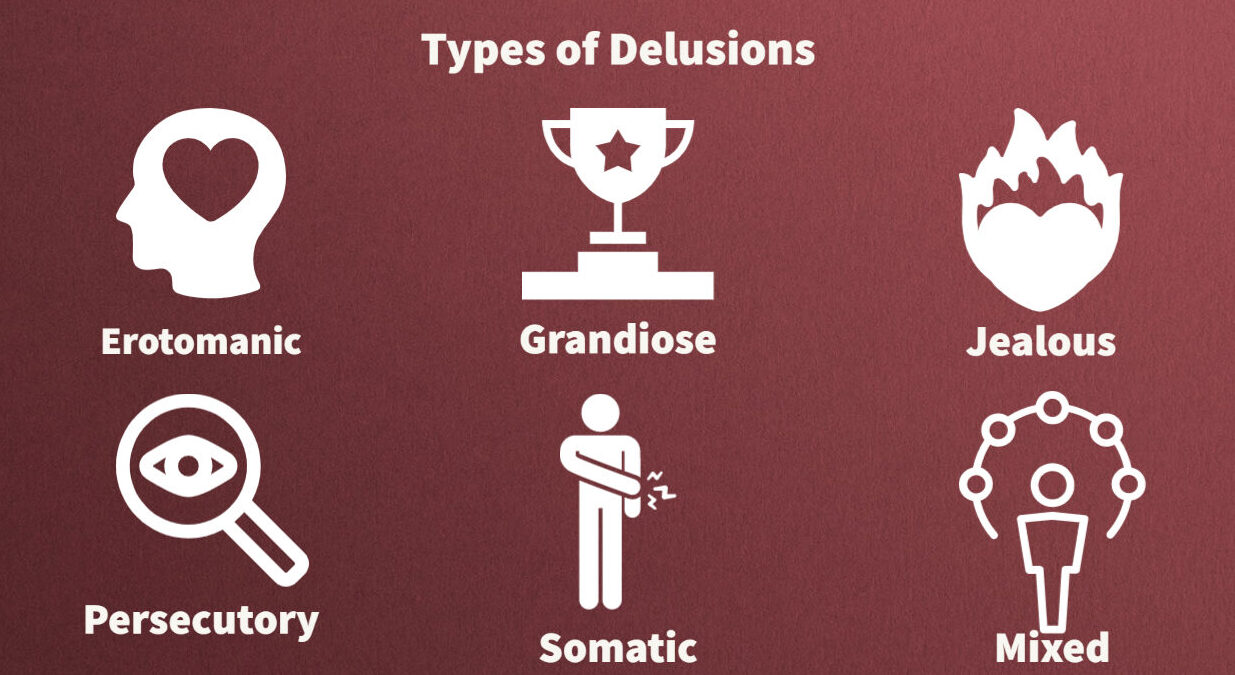
The type of delusional disorder is based on the main theme of the delusions being experienced.
It’s important to note that the below delusions are just some of the many types that exist and that delusions can vary in intensity, frequency, and duration depending on the individual and their specific circumstances.
Erotomanic
This type of delusion is the belief that someone, usually someone who is famous or of a higher social status, is in love with the individual. For instance, the person experiencing this delusion may believe that the famous person is communicating secret messages to them on the TV show they star in.
Stalking behavior is often common with this type of delusion, as the individual may attempt to make contact with the person they believe loves them.
Grandiose
This delusion is the belief that the individual has an over-inflated sense of worth, knowledge, wealth, talent, power, or fame, despite a lack of evidence.
Grandiose delusions involve believing that the individual has special powers, abilities, or a special relationship with a deity or celebrity.
For instance, someone with grandiose delusions may believe they have made an important discovery or were sent by a religious entity to save the world.
Persecutory
This delusion is the belief that the individual, or someone close to them, is being spied on, followed, drugged, cheated on, or mistreated.
They may believe someone is planning to harm them or someone close to them and thus may repeatedly complain to legal authorities.
Jealous
This type of delusion is the belief that a romantic partner or spouse is being unfaithful, despite a lack of evidence to prove this.
The individual may believe their partner is meeting their secret lover whenever not in their presence or is sending their secret lover messages.
Somatic
This delusion is the belief that the individual is experiencing physical sensations, bodily dysfunctions, or suffering from a medical condition.
For instance, they may be convinced that they have a rare illness or parasites living underneath their skin, despite no evidence of this being the case.
Mixed
When the delusions being experienced do not fall into a single category, or there are two or more types of delusions being experienced, this would be labeled as having mixed or unspecified types of delusions.
Causes and Risk Factors
Although there is currently no concrete explanation for what causes delusions, researchers have some ideas as to potential causes or risk factors which may contribute to the onset of delusions.
Genetics
Genetics may play a part in someone developing delusions since it is more common that those with family members with a psychotic disorder with delusions are likely to develop delusions themselves.
For instance, a parent with a delusional disorder or schizophrenia is more likely to have a child who also develops one of these conditions.
Sensory impairments
Delusional disorder tends to be more common among those with impaired vision or hearing.
If someone has problems with vision or hearing, they may be more likely to rely upon inaccurate perceptions of reality if they are less able to see things for how they are, although this is not the case for most of those with these impairments.
This is not to say that everyone with sensory impairments will experience delusions, and not everyone with delusional disorder also has sensory impairments.
Biological causes
There could also be some biological causes that produce the onset of delusions. Joyce (2018) investigated the pathobiology of delusions using case studies of patients who had experienced strokes.
It was found that some of those who had focal strokes to the right lateral prefrontal cortex developed delusions. This part of the brain is known to have connections to the basal ganglia and the limbic system and receive input from the midbrain dopamine neurons.
Dopamine is a neurotransmitter that plays a role in motivation, pleasure, and reward. Dysregulated dopamine has been found to have associations with schizophrenia and those at risk of psychosis, thus suggesting that faulty dopamine signaling could be a precursor of delusion formation.
A further study by Devinsky (2009) found significant associations between the bilateral frontal lobe and delusions in the right cerebral hemisphere.
Damage to this area, a brain region that controls perceptions and thinking, can result in left hemispheric overactivity. The researchers suggested this can result in the left language centers ‘creating a story’ which cannot be compared to reality, corrected, and self-monitored due to damage on the right side.
This can, therefore be confused for reality, and delusional resistance can occur.
Environmental factors
Some environmental factors may contribute to the development or exacerbation of delusions, e.g.,
- Stressful life events: Experiencing traumatic or stressful events, such as abuse, violence, or loss, may increase the risk of developing delusions.
- Social isolation: Lack of social support and social isolation may contribute to the development of delusions, as individuals who are socially isolated may be more prone to feelings of paranoia and mistrust.
- Substance use: Substance use, particularly drugs like amphetamines or hallucinogens, can trigger delusions in some individuals.
It’s important to note that while these environmental factors may contribute to the development of delusions, they do not necessarily cause delusions on their own.
Other conditions
A study by Nygaard, Sonne, and Carlsson (2017) found that a significant number of those who developed posttraumatic stress disorder (PTSD) also developed delusions, specifically of the persecutory type.
Although not the case for most people who have PTSD, this implies there could be a causal link between trauma and stress with the onset of delusions.
As well as delusional disorder, delusions could be a symptom that is triggered by another mental health condition, such as:
- Dementia
- Mood disorders
- Parkinson’s Disease
- Schizophrenia
- Postpartum psychosis
- Substance-induced psychotic disorder
Attributional Biases
Research has also investigated attributional biases in relation to delusion formation and maintenance (Humphreys & Barrowclough, 2010).
This refers to a tendency to make internal attributions for positive events (assigning causality to oneself) but external attributions for negative events (blaming outside causes).
Studies have found this exaggerated self-serving attributional bias exists in some individuals with persecutory delusions, perhaps as a way to protect self-esteem (Bentall, 2019).
However, later research challenges whether this bias is specific to delusions or part of more general coping strategies in psychosis (Humphreys & Barrowclough, 2010).
Reviews also highlight inconsistencies in findings, limited by issues with attributional style measures used across studies (Zhu et al., 2017).
While attributional biases may relate to delusions for some patients, the associations found are not definitive. More research is needed examining both overt and covert attributional tendencies using robust methodology.
Addressing attributional biases could still inform interventions, helping patients modify their reasoning styles.
How To Manage Delusions
Considerations
Understanding and addressing delusions can be a challenging process, especially if the individual experiencing them does not recognize that their beliefs are not based on reality.
It is important to note that some individuals with delusions may resist seeking treatment, making initial treatment difficult.
In cases where delusions do not significantly disrupt everyday life, individuals may not believe that treatment is necessary. In such cases, a gentle and supportive approach by loved ones may be helpful in encouraging the individual to seek treatment, particularly if their delusions are putting them at risk.
Overall, it’s important to approach individuals experiencing delusions with compassion and understanding, and to work collaboratively with mental health professionals to develop a treatment plan that best supports their well-being.
Treatment for delusions can involve medication and psychotherapy.
Medications
The main type of medication recommended is antipsychotics. These have shown effectiveness in that many people with delusions who take antipsychotics showed partial improvement to their symptoms.
Typical antipsychotics are medications that are used to block the dopamine receptors in the brain, which is a chemical believed to be involved in the development of delusions.
These have been used to treat mental health conditions since the 1950s, and some of these include:
- Chlorpromazine (Thorazine)
- Fluphenazine (Prolixin)
- Thiothixene (Navane)
- Perphenazine (Trilafon)
- Haloperidol (Haldol)
- Trifluoperazine (Stelazine)
Atypical antipsychotics are a newer type of medication that are also used to treat delusional disorders but with fewer side effects than the typical antipsychotics.
These work by blocking dopamine and serotonin receptors in the brain and appear to be more effective in treating the symptoms of delusional disorder. Some of these medications include
- Clozapine (Clozaril)
- Aripiprazole (Abilify)
- Asenapine (Saphris)
- Iloperidone (Fanapt)
- Risperidone (Risperdal)
- Olanzapine (Zyprexa)
- Cariprazine (Vraylar)
- Ziprasidone (Geodon)
Some other medications which may be used to treat delusional disorder are antidepressants and tranquilizers.
Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) can be used to treat the depressed or anxious feelings experienced alongside the delusions.
Tranquilizers may be used with individuals who are experiencing very high levels of anxiety or are having trouble sleeping due to the delusions being experienced.
However, care must be taken with medications as they each come with side effects and should only be used if prescribed by a professional.
Psychotherapy
Finally, psychotherapy can also be helpful alongside medications or on its own to help individuals manage and cope with the stress that goes alongside their delusions.
There are several types of psychotherapy that can be used to treat delusional disorder. Here are a few examples:
- Cognitive-behavioral therapy (CBT): CBT is a type of therapy that focuses on identifying and challenging unhelpful thought patterns and behaviors. In the case of delusional disorder, CBT may be effective in challenging and modifying the individual’s delusional beliefs (Sitko et al., 2020).
- Psychodynamic therapy: Psychodynamic therapy focuses on exploring and addressing unconscious patterns of thought and behavior. In the case of delusional disorder, psychodynamic therapy may be used to explore the underlying emotional and psychological factors contributing to developing and maintaining delusions.
- Family Therapy: Family therapy involves working with the individual and their family members to address interpersonal dynamics and communication patterns that may contribute to the individual’s delusions.
- Group therapy: Group therapy involves working with a group of individuals who have similar experiences or challenges. In the case of delusional disorder, group therapy may provide a supportive and validating environment for individuals to explore and process their experiences.
- Acceptance and commitment therapy (ACT): uses acceptance and mindfulness strategies along with commitment and behavior change processes to increase psychological flexibility. Research has shown ACT to be effective in managing psychotic symptoms (Burhan & Karadere, 2021).
It’s important to note that the most effective type of therapy for delusional disorder may vary depending on the individual and their specific needs and circumstances. A mental health professional can work with the individual to develop a personalized treatment plan that best supports their well-being.
Coping Skills for Delusions
Aside from formal therapy, developing coping skills can help those struggling with delusions manage difficult symptoms.
Useful skills include mindfulness to ground oneself in the present; emotion regulation tactics like deep breathing; balancing enjoyable activities; carrying a safety plan for when delusions worsen; peer support groups to reduce isolation; asking loved ones for reality-testing; self-care through healthy routines; and practicing self-compassion.
While delusions persist, building one’s coping toolbox can mitigate their disruption and distress.
Mindfulness helps you remain anchored in the moment when delusions threaten to overwhelm you. Self-care provides stability when symptoms fluctuate. Research suggests that mindfulness-based interventions may reduce delusional symptoms in some (Ellett, 2023).
Peer support reduces feelings of loneliness and alienation. Loved ones can provide objective feedback without judgment.
With time and practice, these skills become valuable lifelong resources for resilience. Even if delusions continue, coping strategies allow one to pursue meaning despite the challenges.
Do you or a loved one need mental health support?
USA
Contact the National Suicide Prevention Lifeline for support and assistance from a trained counselor. If you or a loved one are in immediate danger: https://suicidepreventionlifeline.org/
1-800-273-8255
UK
Contact the Samaritans for support and assistance from a trained counselor: https://www.samaritans.org/; email jo@samaritans.org .
Available 24 hours a day, 365 days a year (this number is FREE to call):
116-123
Rethink Mental Illness: rethink.org
0300 5000 927
References
Bentall, R. P. (2019). Cognitive biases and abnormal beliefs: Towards a model of persecutory delusions. The neuropsychology of schizophrenia, 337-360.
Burhan, H. Ş., & Karadere, E. (2021). Effectiveness of Acceptance and Commitment Therapy for Patients with Psychosis Being Monitored at a Community Mental Health Center: A Six-Month Follow-up Study. Alpha Psychiatry, 22(4), 206.
Devinsky, O. (2009). Delusional misidentifications and duplications: right brain lesions, left brain delusions. Neurology, 72(1), 80-87.
Drake, M. E. (n.d.). Delusional Disorder DSM-5 297.1 (F22). Theravive. Retrieved 2021, August 18, from: https://www.theravive.com/therapedia/delusional-disorder-dsm–5-297.1-(f22)
Ellett, L. (2023). Mindfulness for psychosis: Current evidence, unanswered questions and future directions. Psychology and Psychotherapy: Therapy, Research and Practice.
Humphreys, L., & Barrowclough, C. (2010). Attributional style, defensive functioning and persecutory delusions: Symptom-specific or general coping strategy? The British Journal of Clinical Psychology, 49(2), 231–246.
Joseph, S. M., & Siddiqui, W. (2023). Delusional disorder. In StatPearls [Internet]. StatPearls Publishing.
Joyce, E. M. (2018). Organic psychosis: the pathobiology and treatment of delusions. CNS neuroscience & therapeutics, 24(7), 598-603.
Kalayasiri, R., Kraijak, K., Mutirangura, A., & Maes, M. (2019). Paranoid schizophrenia and methamphetamine-induced paranoia are both characterized by a similar LINE-1 partial methylation profile, which is more pronounced in paranoid schizophrenia. Schizophrenia research, 208, 221-227.
Nygaard, M., Sonne, C., & Carlsson, J. (2017). Secondary psychotic features in refugees diagnosed with post-traumatic stress disorder: a retrospective cohort study. BMC psychiatry, 17(1), 1-11.
Sitko, K., Bewick, B. M., Owens, D., & Masterson, C. (2020). Meta-analysis and meta-regression of cognitive behavioral therapy for psychosis (CBTp) across time: the effectiveness of CBTp has improved for delusions. Schizophrenia Bulletin Open, 1(1), sgaa023.
Zhu, C., Sun, X., & So, S. H. W. (2017). Associations between belief inflexibility and dimensions of delusions: A meta-analytic review of two approaches to assessing belief flexibility. British Journal of Clinical Psychology, 56(1), 59–81.

