Rowsell, M., & Francis, S. E. (2015). OCD subtypes: Which, if any, are valid?. Clinical Psychology: Science and Practice, 22(4), 414.
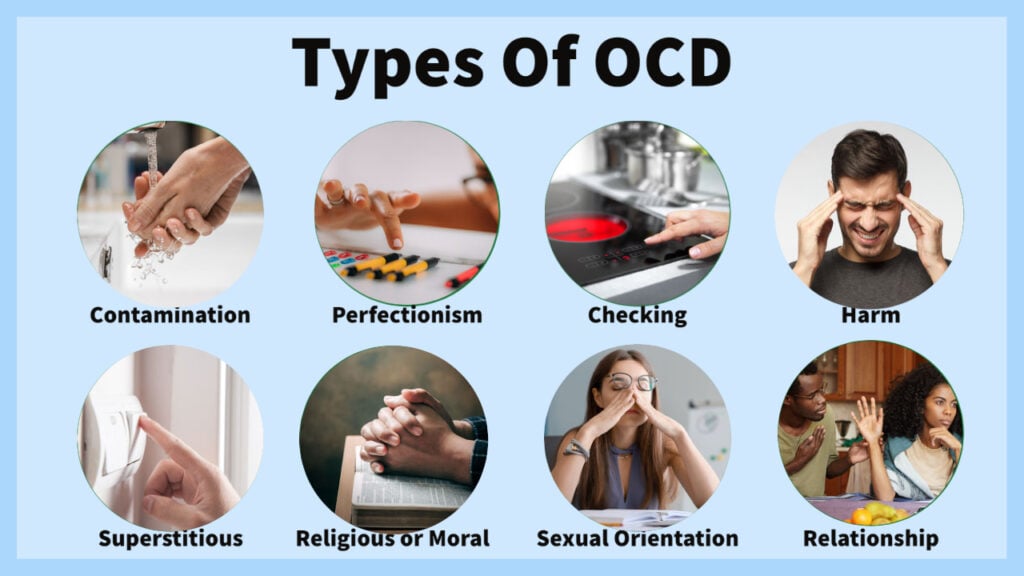
Obsessive-compulsive disorder (OCD) is a heterogeneous mental health condition, with a lifetime prevalence of 2.3% (Kessler et al., 2012). Attempts have been made to subtype OCD to better understand and treat its heterogeneity with subtypes proposed based on features like symptoms, dysfunctional beliefs, and comorbidities (Radomsky & Taylor, 2005).
However, no dominant model fully explains OCD’s heterogeneity across all individuals (Taylor, McKay & Abramowitz, 2005).
This review assessed the validity of proposed OCD subtypes using guidelines set out by Robins and Guze (1970), widely used in psychiatry to develop diagnostic subtypes.
An additional treatment response guideline was included to assess if subtypes had differential treatment outcomes. Understanding valid OCD subtypes could aid with classification, understanding, and specialized treatment of OCD.
Key Points
- The purpose of this review was to assess the validity of proposed OCD subtypes using six guidelines:
- Clinical description
- Treatment response
- Follow-up studies (long-term course)
- Laboratory studies
- Family history
- Delimitation from other disorders
- None of the 21 examined OCD subtypes met all six validity guidelines. The obsession type subtype met five guidelines, while the impulsive, familial, depressive, poor insight, and symmetry/ordering subtypes met four guidelines each.
- The obsession type subtype differentiated between autogenous obsessions (unrealistic and aggressive) and reactive obsessions (realistic and triggered by external stimuli). This subtype met all studied guidelines and shows promise as a valid OCD subtype.
- Three subtypes – poor insight, co-occurring impulsivity, and reactive obsessions – responded significantly worse to first-line OCD treatments, indicating the need for alternate treatment options.
Method
Literature searches were conducted using PsycInfo, PubMed, and Scopus using search terms combining “obsessive-compulsive disorder” and “subtype,” “subclass,” or “subgroup.”
The searches yielded 2181 total studies. Inclusion criteria limited studies to those examining proposed OCD subtypes in relation to at least one validity guideline in adults diagnosed using DSM-IV criteria. 165 unique studies covering 31 putative subtypes were identified.
Statistical Analysis
Guidelines were coded as “studied and met,” “studied and not met,” “not studied,” or “inconsistent” for each subtype.
Subtypes were ranked by number of guidelines met and whether unmet guidelines resulted from insufficient research or not being met despite research.
Results
The researchers reviewed 21 potential subtypes of OCD to see if they could be considered valid. They tested whether each subtype was different from regular OCD in 6 key ways:
- Symptoms (clinical description)
- Response to treatment
- Long-term pattern (follow-up studies)
- Brain differences (laboratory studies)
- Family history
- Clearly different disorder (delimitation)
The researchers found:
- No subtype was clearly valid in all 6 categories tested
- 1 subtype, dividing OCD by type of obsessions (autogenous vs reactive), was valid in 5 categories
- 5 other subtypes were valid in 4 categories:
- OCD with impulsiveness
- OCD running in families
- OCD with depression
- OCD with lack of insight
- OCD with symmetry/ordering symptoms
- Most subtypes were only valid in 2 or 3 categories
- For most subtypes, the categories weren’t met because research showed they were invalid, not just because there wasn’t enough research
Subtypes Meeting 3 Criteria
- Dysfunctional Beliefs (High vs Low)
- Somatic Symptom Themes
- Early vs. Late Onset
- OCD with Trauma
- OCD with Schizotypal Features
- OCD with Obsessive Compulsive Personality Disorder
- Hoarding Symptom Themes
Subtypes Meeting 2 Criteria
- Perfectionism and Certainty Beliefs
- Importance/Control of Thoughts Beliefs
- Responsibility and Threat Beliefs
- Contamination/Washing
- Checking Compulsions
- Purely Obsessional
- Gender Differences
This means:
- The reviewed subtypes likely don’t fully explain the differences seen in OCD
- Dividing OCD by obsession type shows the most promise
- New ways of subtyping may better capture OCD diversity
- Matching treatments to specific subgroups warrants further research
The evidence does not clearly support the validity of most proposed OCD subtypes based on the thorough analysis criteria used in this review.
While the obsession type shows promise, better models for subclassifying OCD are still needed to improve treatment matching and outcomes.
Insight
The review indicates currently proposed OCD subtypes lack clear validity when assessed on multiple key criteria. This likely results from suboptimal categorical subtyping approaches rather than insufficient research into most subtypes.
The obsession type subtype shows the most promise as a valid subtype, possibly due its broader subtype classification compared to other symptom-based subtypes.
Obsession type
The obsession type subtype refers to categorizing obsessive-compulsive disorder (OCD) cases based on the predominant type of obsessions experienced. This subtype divides obsessions into two categories:
- Autogenous obsessions: These are obsessions that are relatively unrealistic, aggressive, or sexual in nature. Common themes include violence, harm, inappropriate sexual behavior or desires, and morality/scrupulosity obsessions.
- Reactive obsessions: These obsessions are more realistic and triggered by external stimuli in the environment. Common reactive obsessions surround contamination, illness/injury, mistakes/accidents, symmetry/order, and hoarding.
The obsession type subtype met 5 of the 6 validity guidelines assessed in the reviewed paper. Cases were assigned to categories based on the individual’s predominant obsession theme.
This subtype shows promise in explaining differences seen in OCD. The autogenous and reactive groups differed significantly in clinical presentation, treatment response, long-term course, laboratory study findings, and delimitation from other disorders.
This suggests tracking obsession themes could aid understanding and specialized treatment of OCD cases.
Strengths
- Rigorously examined multiple proposed subtypes against gold standard validity criteria
- Included less studied criteria like follow-up and family studies
- Highlighted most and least valid proposed OCD subtypes to inform future research
Limitations
- Inconsistent subtype definitions across studies reduces reliability
- Did not quantitatively analyze magnitude of effects in each study
- Did not include pediatric OCD subtypes
- Did not exhaustively search all literature sources
Implications
Dimensional Approaches
The lack of clear discrete subtypes supports the hypothesis that OCD heterogeneity is better captured dimensionally.
Rather than forcing categorical groups, we should measure multiple continuous factors like symptom dimensions, comorbidities, cognitions, etc. concurrently.
This dimensional approach, combined with data analytics, could better explain variance and guide personalized treatments.
Personalized Medicine
Though validity is still unsure, findings reacted meaningful clinical differences between subgroups, like worse treatment response for reactive obsessions. This suggests enough promise to warrant exploratory trials tailoring treatment by OCD subtype, especially for poor prognosis variants.
We have enough data to hypothesize personalized approaches may improve outcomes.
Promising Subtypes
The obsession-type subtype still shows the most empirical promise on validity criteria. Further research should continue to replicate and extend our understanding of autogenous vs reactive presentation.
Examining their cognitive-behavioral processes, neural correlates, genetics, and family history, could reveal meaningful differences to guide treatment.
Beyond obsession type, understudied criteria like family history, course, treatment response should be extended to other promising subtypes like impulsive or poor insight OCD. Broader study on the least established validity criteria for most subtypes is warranted.
Limit Symptom-Based Subtyping
Conversely, the bulk of research exists exploring symptom dimensions like contamination, hoarding, etc. But analyses indicated these fail validity despite extensive study.
The field should limit further efforts to validate these specific symptom presentations. Rather, shift focus to ideological dimensions like beliefs, internal phenomenon like ego-dystonia, and new data-driven approaches.
References
Primary reference
Rowsell, M., & Francis, S. E. (2015). OCD subtypes: Which, if any, are valid?. Clinical Psychology: Science and Practice, 22(4), 414.
Other references
Calamari, J. E., Wiegartz, P. S., Riemann, B. C., Cohen, R. J., Greer, A., Jacobi, D. M., Jahn, S. C., & Carmin, C. (2004). Obsessive-compulsive disorder subtypes: An attempted replication and extension of a symptom-based taxonomy. Behaviour Research and Therapy, 42(6), 647–670. https://doi.org/10.1016/S0005-7967(03)00173-6
Haslam, N., Williams, B. J., Kyrios, M., McKay, D., & Taylor, S. (2005). Subtyping obsessive-compulsive disorder: A taxometric analysis. Behavior Therapy, 36(4), 381–391. https://doi.org/10.1016/s0005-7894(05)80120-0
Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Wittchen, H. (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. https://doi.org/10.1002/mpr.1359
Olatunji, B. O., Williams, B. J., Haslam, N., Abramowitz, J. S., & Tolin, D. F. (2008). The latent structure of obsessive-compulsive symptoms: A taxometric study. Depression and Anxiety, 25(11), 956–968. https://doi.org/10.1002/da.20387
Radomsky, A. S., & Taylor, S. (2005). Subtyping OCD: Prospects and problems. Behavior Therapy, 36(4), 371–379. https://doi.org/10.1016/j.beth.2005.07.003
Robins, E., & Guze, S. B. (1970). Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. The American Journal of Psychiatry, 126(7), 983–987. https://doi.org/10.1176/ajp.126.7.983
Taylor, S., McKay, D., & Abramowitz, J. S. (2005). Is obsessive–compulsive disorder a disturbance of security motivation? Psychological Review, 112(3), 658–656. https://doi.org/10.1037/0033-295x.112.3.650
Keep Learning
Some questions for further discussion:
- If OCD exists on a continuum rather than in discrete categories, how might we best capture and validate the key dimensions of variance?
- Could a personalized medicine approach matching treatments to specific poor prognosis OCD subtypes improve outcomes even in the absence of clearly validated categorizations?
- What benefits and limitations exist with retrospective versus prospective methodologies when studying the longitudinal course of OCD? How might future research address these?
- Why have family studies and treatment response been less studied across proposed subtypes and what implications could focusing research in these areas have?
- Could taxometric analyses inform a more empirically grounded model for understanding heterogeneity in OCD? What other techniques may complement this?

