Generalized anxiety disorder (GAD) is a persistent and common anxiety disorder characterized by excessive, uncontrollable worry about various life events and activities.
Individuals with GAD often struggle with restlessness, fatigue, irritability, muscle tension, and sleep difficulties, alongside their tendency to catastrophize and ruminate. Going through daily life feels emotionally draining or overwhelming.
Getting treatment for GAD is important because the constant state of worry, anxiety, and physiological arousal causes significant life impairment for those with moderate to severe GAD by disrupting relationships, work productivity, and overall well-being.
Fortunately, research supports using both psychotherapy and medication interventions to effectively improve GAD symptoms like chronic apprehension, somatic distress, and functional disability for many patients.

This article outlines recommended first-line treatments for managing generalized anxiety disorder across psychotherapy, pharmacotherapy, and self-help approaches.
Please note that this article should only be used as a general overview of some of the types of treatment options and should not be taken as medical advice. Please see a medical professional if you are considering treatment for GAD.
Medication
Several types of medications are commonly used to treat generalized anxiety disorder (GAD). These include antidepressants, anti-anxiety medications, and anticonvulsants.
Selective serotonin reuptake inhibitors (SSRIs)
Selective serotonin reuptake inhibitors (SSRIs) like escitalopram, paroxetine, and sertraline are a first-line treatment for GAD.
SSRIs work by blocking the reabsorption (reuptake) of serotonin in the brain, leading to higher serotonin levels, which can improve mood and anxiety symptoms.
Randomized placebo-controlled trials show that SSRIs like escitalopram, paroxetine, and sertraline have overall response rates around 60-75% in treating generalized anxiety disorder, compared to 40-60% response rates for placebo.
Potential adverse effects:
SSRIs may cause side effects such as headache, nausea, sleep issues, sexual problems, and activation symptoms.
Serotonin-norepinephrine reuptake inhibitors (SNRIs)
Serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine and venlafaxine also inhibit the reuptake of serotonin and norepinephrine.
Several studies demonstrate the efficacy of duloxetine and venlafaxine XR for acute and long-term treatment of GAD.
Potential adverse effects:
They can potentially lead to side effects such as nausea, sweating, constipation, increased blood pressure, and sexual dysfunction.
Pregabalin (an anticonvulsant)
The anticonvulsant pregabalin binds to calcium channels and reduces neurotransmitter release.
Randomized controlled trials and meta-analyses indicate pregabalin is efficacious and well-tolerated for acute and maintenance treatment of GAD.
Potential adverse effects:
Pregabalin is often well-tolerated but may elicit side effects like blurred vision, weight gain, swelling, and sleepiness.
Benzodiazepines
Benzodiazepines like alprazolam, clonazepam, and lorazepam activate GABA receptors, inhibiting neuron activity.
Benzodiazepines can provide rapid relief from anxiety but are only recommended for short-term treatment of GAD due to risks like dependence and abuse.
Potential adverse effects:
They can confer risks of dependence and abuse. Sedation, memory issues, and coordination problems are also possible side effects.
Medications summary:
First-line recommendations for GAD treatment emphasize SSRIs, SNRIs, and pregabalin, with optimal treatment duration of at least 6-18 months to prevent relapse. Benzodiazepines may be used short-term or as-needed.
Overall, medications can effectively reduce anxiety symptoms and improve functioning in many patients with GAD.
Before considering medication options, please discuss your options and the full side effects with a health professional. This article is meant only as a summary of medications and should not be taken as medical advice.
Psychotherapy
Cognitive-behavioral therapy
Cognitive-behavioral therapy (CBT) is considered the gold standard psychological treatment for GAD. CBT aims to modify habitual, rigid worry patterns by teaching new skills to develop more versatile, relaxed mindsets that minimize anxiety.
The core CBT components include:
Self-Monitoring
Clients track internal cues (thoughts, physical sensations), external triggers, and reactions to understand personal worry patterns and catch early signals of anxiety spirals.
Relaxation Techniques
Methods like slowed breathing, progressive muscle relaxation, guided imagery, and meditation strengthen parasympathetic nervous system tone to induce calmness. These are deployed promptly when detecting worry cues.
Imagery Training
Visualizing pleasant scenes promotes relaxation as an alternative to verbal-linguistic worry.
Cognitive Restructuring
Identifying and challenging irrational assumptions, logical errors, and the tendency to catastrophize counteracts worrying. Behavioral experiments test anxious predictions.
Self-Control Desensitization
Visualizing coping with worry triggers facilitates fear tolerance through corrective learning rather than avoiding feared imagery.
Other elements like mindfulness, intolerance of uncertainty approaches, and emotion regulation skills may supplement traditional CBT.
Benefits include reduced threat appraisals, attentional/interpretive biases, autonomic hyperarousal, and somatic tension. Potential challenges involve compliance with self-monitoring, practicing new skills, and accepting the necessity of distress tolerance.
Overall, 50-60% of GAD patients attain remission after CBT, with gains maintained long-term. Future research can clarify optimal treatment matching and subcomponents for diverse clinical profiles.
Acceptance and Commitment Therapy
Acceptance and commitment therapy (ACT) is a type of psychotherapy that aims to help people live better with uncomfortable feelings and experiences related to their anxiety rather than trying to get rid of them.
ACT for anxiety focuses on:
- Acceptance – Learning not to fight against anxiety symptoms but to make room for them instead. This is because efforts to control or eliminate anxiety often backfire and make it worse.
- Mindfulness – Being fully present in each moment with curiosity and without judgment, including during times of anxiety or worry. This helps reduce struggle and suffering.
- Values – Clarifying what gives life meaning and purpose for each person. Values are chosen directions that guide actions, even during difficult emotions.
- Committed action – Setting goals and carrying out behaviors aligned with values, while willingness accepting uncomfortable internal experiences that show up.
Research shows ACT can lower symptoms of anxiety and depression and increase quality of life in conditions like chronic pain and multiple anxiety disorders.
Although more research is still needed, early trials also suggest ACT may help older adults specifically. Studies found it reduced worry, anxiety, and depression and improved treatment completion rates compared to traditional cognitive behavior therapy (CBT).
By focusing less on controlling anxiety and more on valued living, ACT offers an alternative approach to treating persistent GAD that warrants further research in this population.
Emotion-Focused Therapy
Emotion-focused therapy (EFT) is an experiential, humanistic approach that views anxiety and worry in GAD as attempts to protect the self from being overwhelmed by painful emotions that the person cannot soothe on their own.
- Transforming maladaptive emotions like fear, sadness and shame resulting from early attachment injuries, trauma or emotional invalidation
- Teaching emotion regulation skills
- Instilling more positive, self-compassionate ways of relating to feelings and needs
Through empathic exploration of personal narratives, EFT helps individuals symbolize suppressed experiences causing distress and understand negative self-treatment patterns learned when emotions were dismissed or silenced.
Therapists facilitate “two-chair dialogues” to resolve anxiety splits between a worrying part and an overwhelmed experiencer. Further chairwork accesses core painful feelings, undoes self-invalidation, and develops self-soothing capacities.
EFT has demonstrated effectiveness for GAD in multiple case studies and some randomized trials. A 2009 study found interventions evoking clients’ emotions and bodily feelings were most helpful reported by patients.
Subsequent research confirms techniques like focusing, validating emotional experience, and transforming maladaptive feelings relieve anxiety symptoms and improve life functioning.
Considerations:
- EFT requires a willingness to engage with and process feelings, which may seem overwhelming initially to avoidant clients
- Transformation of attachment injuries and developmental trauma means a longer course of therapy is typically needed
- Lack of sufficient early nurture and secure bonds may complicate forming therapeutic relationship required for modeling self-compassion
With adequate sessions over 6-24 months, EFT fosters confidence, resilience, and skills for regulating distress independently. Further controlled studies would strengthen the evidence base.
Self-Help Techniques
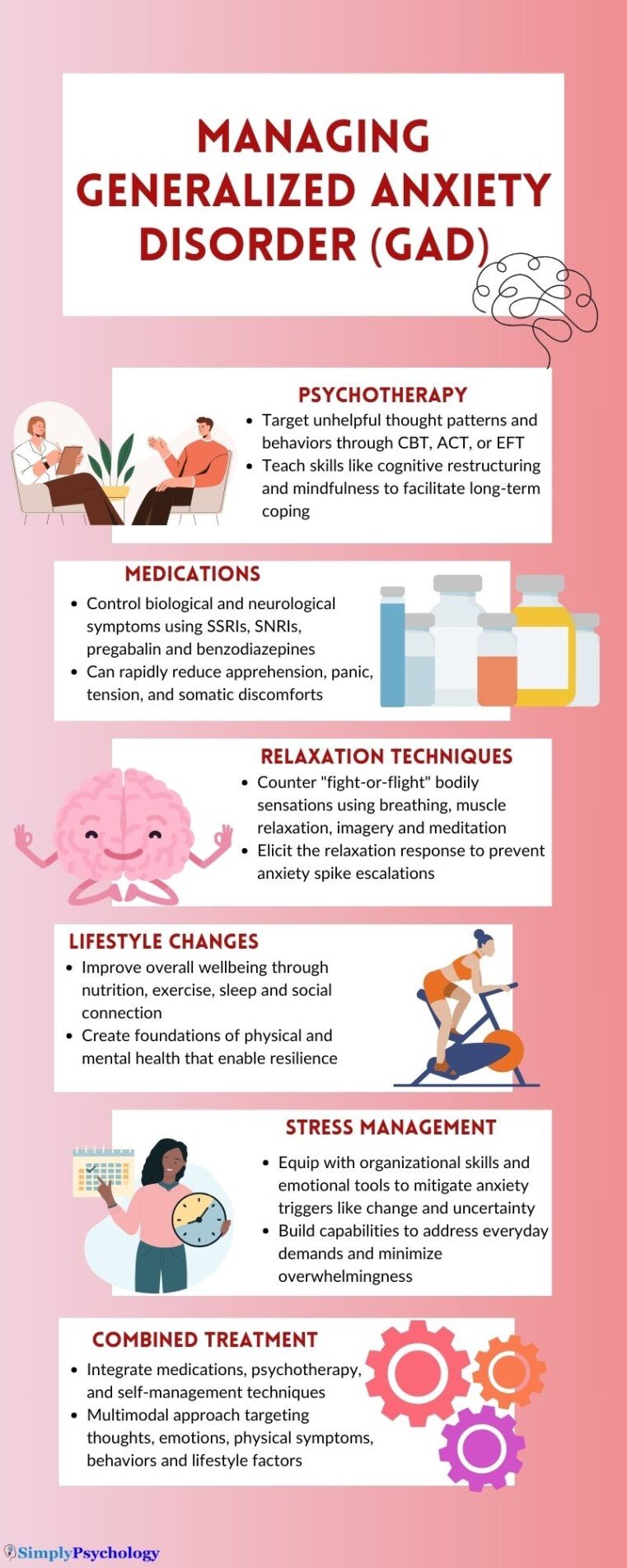
Alongside professional treatment, there are many self-help techniques people with GAD can try to better cope with their anxiety. These involve making positive lifestyle changes, learning stress management skills, using relaxation techniques, and practicing mindfulness.
Some of these techniques can be used as and when anxiety strikes when you need to reduce anxiety quickly, or they may be implemented into your lifestyle as long-term strategies.
Lifestyle Changes
Improving overall physical health and well-being can help create a strong foundation for managing anxiety. This includes:
- Getting regular exercise releases endorphins that improve mood
- Eating a balanced, nutritious diet and staying hydrated
- Getting adequate sleep and maintaining a consistent sleep routine (which can all be very useful when you need to calm anxiety at night)
- Limiting alcohol and avoiding illicit drugs and excessive caffeine
- Making time for enjoyable hobbies and social connection
Stress Management Skills
Learning to mitigate sources of stress can prevent anxiety from intensifying. Useful skills include:
- Organizational strategies – Make daily to-do lists, break down big tasks, declutter to reduce overwhelm.
- Time management – Prioritize important tasks, schedule worrying for set times.
- Problem-solving – Define issues, brainstorm solutions, evaluate options.
- Assertiveness – Express needs and set boundaries diplomatically.
Relaxation Techniques
Techniques that elicit the body’s relaxation response counter “fight-or-flight” sensations. These include:
- Diaphragmatic breathing – Slow, abdominal breathing to relax muscles.
- Progressive muscle relaxation – Tense and release muscle groups.
- Guided imagery – Picture calming scenes in detail using all senses.
- Meditation – Practice mindfulness, self-observation without judgment.
Practicing regularly elicits calmness faster. These can be used whenever anxiety ramps up.
Mindfulness
Mindfulness means focusing awareness on the present moment rather than brooding over the uncertain future. Useful skills include:
- Observing thoughts/emotions without reacting or judging
- Noticing anxiety but letting sensations pass without escalating worry
- Catching catastrophic thinking and refocusing on the current situation
- Accepting, allowing and making room for anxiety when it arises
Using mindfulness, people can learn to step back and dis-identify from anxiety and worry rather than being entangled in attempts to fight it. Apps like Headspace provide guided mindfulness sessions.
Trying various anxiety self-help strategies allows people to determine what works best for them personally in managing symptoms, preventing escalation into panic, and staying grounded in the present.
Conclusion
GAD involves ongoing, unremitting anxiety, tension, and worry, which substantially impacts one’s quality of life and ability to function.
Research supports using both psychotherapy approaches to address maladaptive thoughts and behaviors as well as medications to improve biological anxiety symptoms. Self-help techniques also assist with lifestyle factors, skill building, and coping ahead of escalation.
While GAD remains challenging to treat given high rates of chronicity and comorbidity, the interventions outlined targeting cognitive, emotional, physiological, and behavioral aspects of GAD can increase individuals’ self-efficacy in managing symptoms.
Combining professional modalities like CBT or medication with consistent self-help techniques, including relaxation, organization skills, and mindfulness practices, is recommended for optimal treatment response.
References
Allgulander, C., & Baldwin, D. S. (2013). Pharmacotherapy of generalized anxiety disorder. Modern Trends in Pharmacopsychiatry, 29, 119–127. https://doi.org/10.1159/000351955
A-Tjak, J. G. L., Davis, M. L., Morina, N., Powers, M. B., Smits, J. A. J., & Emmelkamp, P. M. G. (2015). A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychotherapy and Psychosomatics, 84(1), 30–36. https://doi.org/10.1159/000365764
Baldwin, D. S., Ajel, K., Masdrakis, V. G., Nowak, M., & Rafiq, R. (2013). Pregabalin for the treatment of generalized anxiety disorder: an update. Neuropsychiatric disease and treatment, 883-892. 10.2147/NDT.S36453
Baldwin, D. S., Waldman, S., & Allgulander, C. (2011). Evidence-based pharmacological treatment of generalized anxiety disorder. The International Journal of Neuropsychopharmacology, 14(5), 697–710. https://doi.org/10.1017/S1461145710001434
Cuijpers, P., Sijbrandij, M., Koole, S. L., Huibers, M. J., Berking, M., & Andersson, G. (2014). Psychological treatment of generalized anxiety disorder: a meta-analysis. Clinical Psychology Review, 34(2), 130-140. https://doi.org/10.1016/j.cpr.2014.01.002
Davidson, J. R., Wittchen, H. U., Llorca, P. M., Erickson, J., Detke, M., Ball, S. G., & Russell, J. M. (2008). Duloxetine treatment for relapse prevention in adults with generalized anxiety disorder: a double-blind placebo-controlled trial. European Neuropsychopharmacology, 18(9), 673-681. https://doi.org/10.1016/j.euroneuro.2008.05.002
Elliott, R. (2013). Person-centered/experiential psychotherapy for anxiety difficulties: Theory, research and practice. Person-Centered & Experiential Psychotherapies, 12(1), 16-32. https://doi.org/10.1080/14779757.2013.767750
Garakani, A., Murrough, J. W., Freire, R. C., Thom, R. P., Larkin, K., Buono, F. D., & Iosifescu, D. V. (2020). Pharmacotherapy of anxiety disorders: current and emerging treatment options. Frontiers in psychiatry, 1412. https://doi.org/10.3389/fpsyt.2020.595584
Generoso, M. B., Trevizol, A. P., Kasper, S., Cho, H. J., Cordeiro, Q., & Shiozawa, P. (2017). Pregabalin for generalized anxiety disorder: an updated systematic review and meta-analysis. International clinical psychopharmacology, 32(1), 49-55. https://doi.org/10.1097/YIC.0000000000000147
Katzman, M. A., Bleau, P., Blier, P., Chokka, P., Kjernisted, K., Van Ameringen, M., … Walker, J. R. (2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry, 14 Suppl 1(Suppl 1), S1. https://doi.org/10.1186/1471-244X-14-S1-S1
Levy Berg, A., Sandell, R., & Sandahl, C. (2009). Affect-focused body psychotherapy in patients with generalized anxiety disorder: Evaluation of an integrative method. Journal of Psychotherapy Integration, 19(1), 67–85. https://doi.org/10.1037/a0015324
Watson, J. C., & Greenberg, L. S. (2017). Emotion-focused therapy for generalized anxiety. American Psychological Association. https://doi.org/10.1037/0000018-000
Wetherell, J. L., Afari, N., Ayers, C. R., Stoddard, J. A., Ruberg, J., Sorrell, J. T., Liu, L., Patterson, T. L., Thorp, S. R., Golshan, S., Nord, K., & Petkus, A. J. (2011). Acceptance and commitment therapy for generalized anxiety disorder in older adults: a preliminary report. Behavior therapy, 42(1), 127–134. https://doi.org/10.1016/j.beth.2010.07.002
Wilson, A. J., & Stein, D. J. (2019). Pharmacological treatment of anxiety disorders. In S. M. Evans & K. M. Carpenter (Eds.), APA handbook of psychopharmacology (pp. 195–215). American Psychological Association. https://doi.org/10.1037/0000133-009